Effectiveness of Adoptive T-Cell Immunotherapy May Depend on Gut Microbiome
New research suggests that the composition of bacteria in the gastrointestinal tract may help predict which patients with cancer may benefit most from adoptive T-cell immunotherapy (ACT), including chimeric antigen receptor (CAR) T-cell therapy.Reporting recent findings in the Journal of Clinical Investigations and Insights, Mireia Uribe-Herranz, PhD, and colleagues found that the effectiveness of ACT in a mouse model is significantly impacted by differences in the makeup of gut bacteria and that the efficacy of ACT is improved by treatment with orally administered vancomycin, an antibiotic that targets gram-positive bacteria in the gut.
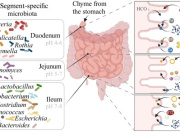
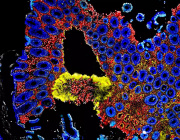
The research team examined the relationship between gut microbiome composition and response to ACT in a mouse model of cervical cancer using female mice from 2 laboratories (Jax and Harlan); previous studies have indicated that mice derived from different vendors can have different gut bacteria despite having an identical genetic makeup, say the authors. The mice received T cells, generated by vaccination of donor mice, 5 days after being implanted with tumors and 7 days after undergoing lymphodepletion.
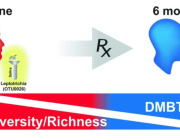
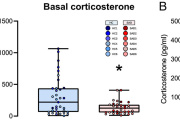
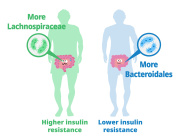
In the mice from the Harlan laboratory, the T-cell transfer resulted in nearly complete tumor growth abrogation (P <.001), but in the mice from the Jax laboratory, the treatment was less effective.To investigate the differences in gut microbiota and whether they could be linked to treatment efficacy, the researchers carried out a gene sequencing of the animals’ stool samples. They found that the Harlan-derived mice had a greater diversity in microbiota of the Bacteroidetes taxa, whereas the Jax mice were dominated by Bacteroidales S24-7 alone.To investigate the relevance of these differences, the researchers treated both sets of mice with antibiotics and found that orally administered vancomycin—which is not absorbed and is therefore limited to the intestine—given 10 days before ACT, depleted bacteria of the Bacteroidetes phylum. After vancomycin treatment, tumor progression was reduced in the Jax mice, whereas no change was observed in the Harlan mice.
Oral vancomycin also increased levels of the cytokine interleukin-12 (IL-12), which the authors say can sustain systemic adoptively transferred antitumor T cells, in the mice. To demonstrate a similar effect in patients, the researchers examined a cohort of patients undergoing ACT for hematologic malignancies. In December 2015, patients in this cohort, all of whom were treated at the University of Pennsylvania, had received vancomycin prophylaxis against Clostridium difficile, which allowed the researchers to compare IL-12 levels in this group with historical controls. The researchers observed an increase in IL-12 levels in the group who received vancomycin, just as they observed in the animal model.
To confirm the role of IL-12 in increasing ACT’s efficacy, the researchers injected a blocking antibody for IL-12 into mice that had been treated with ACT and vancomycin and saw a positive effect on tumor growth and a loss of T-cell infiltration.Like antibiotic treatment, heterologous fecal transfer impacted the efficacy of ACT; when the Harlan mice were given microbiota transfer from the Jax mice, vancomycin therapy replicated the tumor reduction found in the Jax mice.“This means that the microbiota-dependent response to ACT was successfully transferred between mice, and that modulation with specific antibiotics can be used to increase ACT efficacy,” said Andrea Facciabene, PhD, one of the study’s authors, in a statement.The authors say that a better understanding of the mechanisms of the gut microbiome will help to maximize the efficacy of ACT in the future and that the microbiome may need to be modulated in a therapy-specific manner to achieve the greatest treatment efficacy.
News source: http://www.ajmc.com