A PSA from your gut microbes: Enjoy the holidays but don't forget your fiber
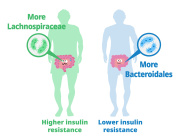
Anyone watching their waistline this holiday season may want to pay attention to what their gut bacteria are eating. It's not just calories that matter in a healthy diet—it's fiber that resists digestion by the body but is readily eaten by bacteria in the gut. The amount of fiber in someone's diet can influence weight gain, blood sugar, insulin sensitivity, and colon health. Two studies with mice, publishing December 21 in the journal Cell Host & Microbe, help shed light on how and why fiber has such a powerful effect on the entire body.
"Once the mechanism is understood, it can be exploited in different ways to promote health," says Andrew Gewirtz, who studies the intestinal epithelium at Georgia State University's Center for Inflammation Immunity & Infection and is senior author of one of the papers. "This will allow ways to modify diets to maximize those benefits."
Fiber in its various forms is found in fruits, legumes, vegetables, and whole grains. So-called Western diets, which are high in fats and sugars but low in fiber, have been linked to an increased risk of inflammatory bowel diseases, weight gain, and diabetes.
"It is becoming increasingly clear that the average person's fiber intake in a Western country has drastically reduced over the past few decades," says Fredrik Bäckhed, who studies the role of the normal gut microbiota in metabolic diseases at the University of Gothenburg, Sweden and is a co-senior author of the other paper.
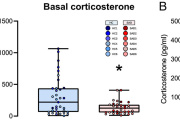
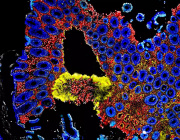
Both studies started by feeding a group of mice a diet that was extremely low in fiber. The low-fiber diets rapidly led to weight gain, high blood sugar, and insulin resistance in the mice. The Bäckhed study found that mice developed problems with the protective mucus layer in the colon after just 3-7 days of eating the low-fiber diet: this mucus layer became more penetrable and bacteria encroached upon the epithelial cells of the colon. The Gewirtz study observed that the colons of mice on the low-fiber diet shrank significantly in thickness. And not only did large amounts of gut bacteria die off after mice ate a low-fiber diet, mice developed unhealthy imbalances of different gut bacteria strains.
"These papers show the importance of the inner mucus layer in separating bacteria and human host. It nicely illustrates how dynamic and quickly this responds to diet and bacterial alterations," says Gunnar C. Hansson, a co-senior author with Bäckhed and a professor in the Mucin Biology Group at the University of Gothenburg, Sweden.
"Both our paper and the Bäckhed paper are essentially reaching the same conclusion that the lack of fiber results in bacteria encroaching into the mucus layer, and those bacteria are promoting low-grade inflammation, contributing to metabolic syndrome," says Gewirtz.
After the fallout from the low-fiber diet, the two research teams tried different treatment approaches.
Bäckhed, Hansson, and colleagues found that a transplant of gut bacteria from a healthy mouse could undo some of the harmful changes to the colon mucus layer. Supplementing the mice with Bifidobacterium (a beneficial bacteria) helped colon mucus growth issues, but not mucus penetrability issues. Supplementing the mice's diet with inulin (a type of fermentable fiber) lowered the mucus penetrability but did not help mucus growth issues.
By switching mice to a diet comprised of 20% inulin, Gewirtz and colleagues found that they could reverse some aspects of metabolic syndrome in the mice—like promoting weight loss and greater blood sugar control—but not others, such as elevated triglycerides levels.
The fiber inulin also helped restore colon mass, increased the number of intestinal absorption cells enterocytes, and restored some number and diversity to the gut bacteria. However, the fiber supplements could not completely return the mouse gut bacteria to its original bacterial diversity after eating the low-fiber diet. This may mean using supplements as a treatment could cause complications if a person doesn't have a healthy mix of gut bacteria.
"Diets that lack fiber alter the bacterial composition and bacterial metabolism, which in turn causes defects to the inner mucus layer and allows bacteria to come close [encroach], something that triggers inflammation and ultimately metabolic disease," says Hansson. "It is not enough just to add fiber to your diet; it also depends on which bacteria you carry."
This likely means more study is needed before fiber supplements can be used as a treatment.
"Simply enriching processed food with purified fibers might offer some health benefits, but we're not ready to recommend it until we understand more of the very complex interplay between food, bacteria, and host," Gewirtz says. Bäckhed and Hansson agree.
News Source: medicalxpress.com